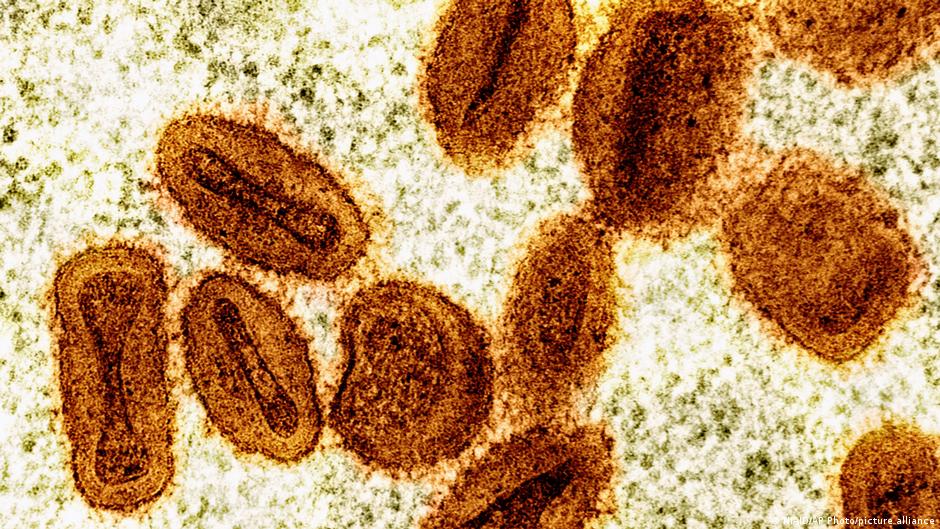
Health officials in the United Kingdom confirmed on December 8, 2025 that they had detected a so-called “recombinant” version of the mpox virus in a male patient.
A virus becomes a recombinant virus when two existing versions of it recombine – combining their genetic information – to form a new, hybrid version. This can happen when different types of viruses infect a person at the same time.
UK National Health Protection Agency, UKHSA says recombinant MPOX virus Found in a person who had recently returned to the UK from Asia.
According to the World Health Organization (WHO), cases of mpox have been recorded in Thailand, Malaysia and Japan in 2025 – making it appear that the case in Japan was imported by someone who returned from a trip to the African country.
Katy Sinka, UKHSA’s head of sexually transmitted infections, and other epidemiological experts said further research would be needed to understand how MPOX is changing globally.
But mPox and other “poxviruses” have been known to mix and create their own new versions.
The evolution of the virus is predictable
Mpox, previously known as “monkeypox”, was originally found in lab monkeys in Denmark in 1958. The first human infection was found in a Congolese child in 1970.
It is related to smallpox and the prevalence of mpox has increased since the eradication of that disease in 1980. Two genetically distinct “clades” of mpox are particularly prevalent in West and Central Africa and parts of Asia. The clade IIb subtype is responsible for the ongoing global outbreak since 2022, primarily affecting Asia, Europe, and the Americas.
Viruses constantly evolve as their genetic code undergoes mutations. This was seen, for example, during the COVID-19 pandemic: new variants of the SARS-CoV-2 virus emerged as it spread around the world.
In this latest case of mpox in the UK, material from clade IB and IIB viruses have combined to form a new hybrid strain.
“If this recombinant was made in human cells, the person would have been infected by both groups simultaneously,” said Jesse Dunning, an infectious disease consultant at the Institute of Epidemiology at the University of Oxford.
“Exposure to two different viruses may not happen simultaneously, but to one,” Dunning said. [m]pox virus infection in someone with a fully functioning immune system, I think the conditions favorable to recombination will be optimal if the two viruses come into contact simultaneously or near together.”
Although there is no indication that this recombinant MPOX virus poses any additional threat, Dunning said it was a timely reminder that MPOX continues to evolve, and its infectiousness may change.
“The expectation – and it is a reasonable expectation – is that a recombinant virus will not transmit as efficiently as the individual ‘component’ viruses, but we need laboratory data, case data and epidemiological data to confirm this,” Dunning said.
What is the global status of mpox infection?
Despite its original association with monkeys, Mpox has been found in various mammals, as well as humans.
This was a global outbreak of human infection, involving clades I and II, leading WHO to declare a public health emergency in August 2024. This is still a major challenge in the Democratic Republic of Congo, which recorded more than 20,000 cases in the first 10 months of 2025.
Following a decline in cases in DR Congo, Sierra Leone, and Burundi, WHO Director-General Tedros Adhanom Ghebreyesus rescinded that order in September 2025, although MPOX still circulates globally.
In humans, mpox is usually spread by contact with infected people. This includes exposure to respiratory particles through skin contact, sexual and mouth-to-mouth contact, and breathing.
Infected mothers can pass the disease to their children during pregnancy or birth. Infection can also be spread through contaminated objects such as needles and clothing.
The primary high-risk group are men who have sex with men (MSM).
Following the latest case in the UK, the government there has also identified people with multiple sex partners, those having group sex and those visiting sex-on-premises venues (SOPVs) as at risk. The UKHSA recommends all such groups to get vaccinated.
The current vaccine is 75–80% effective in protecting against clade II MPox.
Is there a risk of this new MPox strain spreading outside the UK?
At the time of writing it is difficult to say whether this hybrid MPOX will spread outside the UK. But experts suggest it may depend on people’s access to mpox vaccination.
While many countries have good access to the mpox vaccine, parts of Asia and Africa are having difficulty getting the vaccine to those who need it most.
If this does not improve, it will be possible for mPox to continue to evolve and reemerge in areas where transmission of the virus is still high. And new versions, or mutations, of any virus bring with them the risk of being more infectious than previous versions.
“The main concern now is whether this new strain will change the infectivity or virulence of the virus,” said Boghuma Titanji, an infectious disease expert at Emory University in the US. “The more mpox circulation we allow, the more opportunities the virus has to recombine and adapt, the more robust the mpox virus becomes as a human pathogen that is not going away.”
How can I prevent mpox infection?
And while vaccination can help prevent infection, preventive measures are also important.
Experts have emphasized that Mpox infection often causes mild illness and that most people recover in 2–4 weeks. WHO advises infected people to isolate from others and take steps to prevent further infection. These measures include:
- Where possible, stay at home and in a well-ventilated room
- Continue good hygiene practices including hand washing with soap
- keep wounds dry and open when left alone
- Cover wounds and wear a facemask to prevent spreading the virus when near other people
- Avoid touching sores that appear during infection and touching other objects that may be touched by others
- Use over-the-counter pain relievers as prescribed by qualified professionals
- Do not touch or move sores or wounds, as this will prevent healing and may increase the risk of spreading mumps.
Edited by: Zulfikar Abbani





Leave a Reply